Hospital ramping is the hot topic on everyone’s lips. But did you know a whopping $130 million is being injected into virtual healthcare to help free up hospital beds across the state? Here’s why.
Have you heard of virtual care?
Virtual care remotely connects patients with health professionals to deliver care when and where it’s needed. This might be in the form of a phone call, video conference or remote monitoring (using technology to collect and send medical data without having to present in person).
There are two virtual care services: one for children and adolescents and another for adults. Read on to find out more.
Why does it matter?
We’re glad you asked. What virtual care also does – and this is why it matters to all of us – is keep people out of emergency departments if they don’t need to be there. Nearly 80 per cent of SA Virtual Care Service patients avoid admission to hospital emergency departments and instead receive individualised care in place, or via more appropriate services in the community, easing reliance on metropolitan hospital resources.
What support is there for virtual care services?
The Government of South Australia is injecting tens of millions of dollars into two successful virtual health care services:
The Child Adolescent Virtual Urgent Care Service (CAVUCS)
Funding: $30.8 million
Timeline: Over the next four years
How will it help? This is a permanent extension of the popular service that was funded temporarily during Covid. It connects families remotely with a virtual team of highly skilled emergency doctors and nurses at the Adelaide Women’s and Children’s Hospital.
The adult SA Virtual Care Service (SAVCS)
Funding: $67.8 million
Timeline: Over the next five years
How will it help? The SAVCS brings comprehensive care to patients that would normally only be available in an emergency department (ED). SA Ambulance crews, regional clinicians and aged care staff on the scene with a patient work with the service’s senior clinicians via video link, to support an individualised assessment. Started in December 2021, the service cannot currently be contacted directly by patients. The funding will make this service permanent and expand its reach, further helping reduce ED presentations.
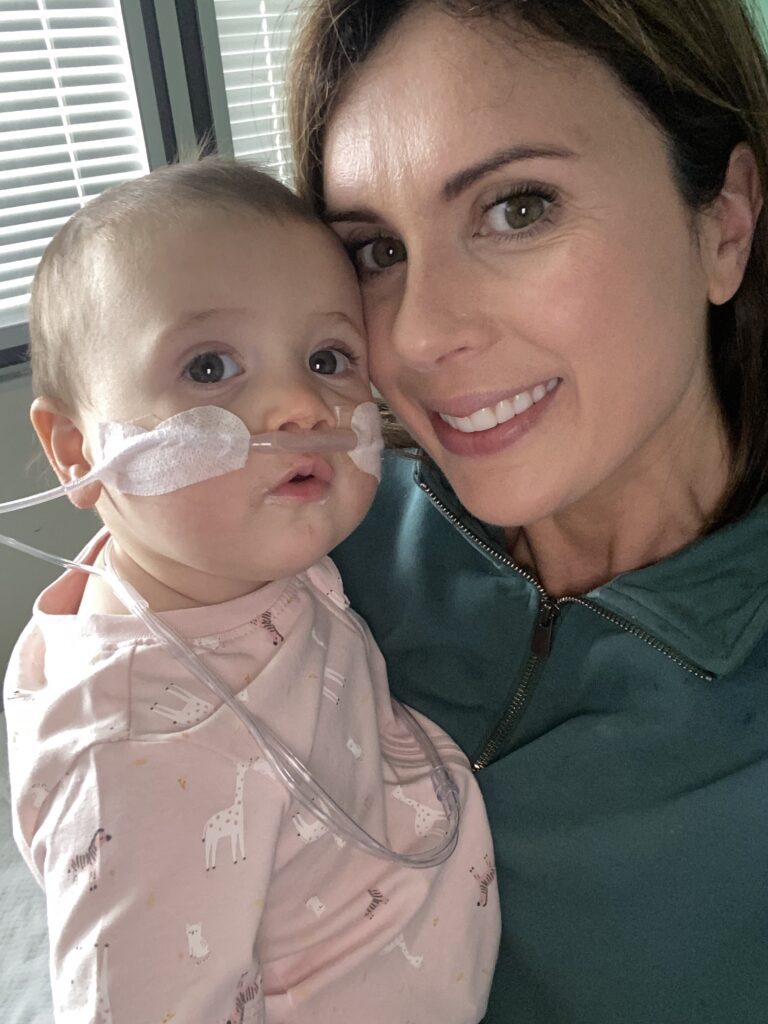
For Kate and her two kids, virtual healthcare has been a literal life saver
When Kate had her first child, Jock (now three), during the pandemic, and then her second child, Claudia (now 18 months), toward the end of lockdowns, the thought of going to hospital didn’t feel like the safest option. It didn’t always feel entirely necessary, either.
For Kate, virtual care services have been both an educational tool in helping her know how to react to signs of illness in her kids (“Do I need to get an ambulance? Can I drive to the hospital? Is there time to wait for a doctor?”), and a first stop in monitoring her daughter’s severe asthma.
As an infant, Jock developed a full-body rash. At the time, she didn’t know about virtual care and so she put in a call to the Women’s and Children’s Hospital and was connected to a health direct line. Despite being told it wasn’t serious and to wait until morning to see a GP, the condition worsened and Jock had a first health assessment by virtual means, which resulted in an ambulance dash to the hospital.
This experience opened Kate’s knowledge of the services available to her as a parent and the value of a virtual option.
Then when her daughter Claudia arrived 18 months later, Kate learnt about the CAVUCS, which allowed her to bypass the initial back-and-forth she had experienced with Jock. Their lives changed for the better.
Kate shares her experience.

“The Women’s and Children’s put me onto an external health care provider, which is more of a general health hotline. I explained (Jock’s) rash to them, and I remember being told, ‘Go and see the GP in the morning’. But the rash got worse, and other symptoms developed,” Kate says.
“I ended up calling the hospital again and insisting on being put through to the emergency department. This felt like the only option at the time as we were in the middle of a lockdown and I didn’t know about virtual care.
“I was connected with an emergency nurse and after answering a few questions, Jock was assessed via teleconference, which was similar to a FaceTime consult.
“The nurse was brilliant; she walked us through all the tests and did triage through the visual call. She promptly organised an ambulance. When we got to the hospital, they were expecting us.”
A few years later, when Claudia presented with her first signs of respiratory distress, Kate came across the details for CAVUCS via a parenting group. It was a more direct path to the service than she had experienced with Jock. With a video function and a qualified nurse and/or doctor at the other end of the line, there was another layer of comfort.
Kate described Claudia’s (then six months) symptoms – which turned out to be Respiratory Syncytial Virus (RSV) – and was told by a doctor to either go straight into the hospital or they would send an ambulance to the home.
Claudia has been in and out of hospital in the year since, and being able to call ahead and speak to a medical professional has saved Kate and her family hours of waiting time and reduced the risk of being exposed to other illnesses.
“I have definitely felt the comfort of being able to call ahead and speak to emergency,” says Kate.
“Previously, you didn’t have the privilege of a direct line to the emergency department’s nurses and doctors. So, the best option was to wait in a long line and sit in the emergency room with very ill children for hours on end. It always felt backwards and inefficient, like you were being told to be quiet and wait your turn.
“There’s a human element to it now. As a family that frequents the Women’s and Children’s, the importance of taking the pressure off the emergency room is so extremely beneficial to the children that are compromised and need immediate attention.”
With growing pressures on the health system and the State Government actively working on solutions to try and ease wait times, Kate says a service like this has undoubtedly contributed to the changes she’s witnessed in emergency.
“The emergency ward has changed, in my opinion. When I had Jock, and even in the early stages of Claudia’s health battles, I would see long lines out the door of the emergency room at the hospital. People were suffering from all different scenarios, from real critical situations to those who may be better suited to a GP clinic,” Kate says.
“It’s really stressful as a parent when you have a child struggling to get oxygen while their tiny chest is heaving but you’re waiting in a line with patients, who are not critical, queuing ahead of you.
“I feel that this service could help unwell but not seriously sick or injured people avoid hospital. The more people that know about virtual care services, the better.”
In addition to providing support in her daughter’s early stages of her illness, virtual care services provided Kate with great comfort. With so many unknowns, particularly during the time of Covid, it was comforting to know she had another option before rushing to an emergency room.
“These services are so important. There’s obviously a lot for first-time parents to know; when something happens, the knee-jerk reaction is always to go into emergency – especially considering it’s so hard to get into a GP in the current climate,” Kate says.
“Virtual care gives people that extra step between visiting a GP and going to the emergency department.
“I am such a supporter of this service because we, as parents, have a right to keep our children safe. If you are in doubt, I highly recommend that you call the line.”